When Trigeminal Neuralgia Strikes
Why attacks differ, what triggers them, and why variability is the rule, not the exception
by Aneeta Prwm MBE
When trigeminal neuralgia strikes, many people expect the pain to behave consistently. They look for the same trigger, the same sensation, and the same pattern each time.
At first glance, that expectation feels reasonable. In reality, however, it is medically incorrect.
Trigeminal neuralgia is an unstable neurological disorder. For that reason, variability is not an anomaly but one of its defining clinical features. When this basic fact is misunderstood, people are doubted, diagnosis is delayed, and unnecessary dental or ENT treatment often follows.
Because of this, understanding why attacks differ when trigeminal neuralgia strikes is central to understanding the condition itself.
When trigeminal neuralgia strikes: what the condition actually is
Trigeminal neuralgia is a cranial neuropathic pain disorder involving dysfunction of the trigeminal nerve, the main sensory nerve of the face. According to the International Headache Society, it is characterised by recurrent, severe facial pain arising from abnormal trigeminal nerve activity.
Crucially, that abnormal activity may be spontaneous or stimulus-evoked. In other words, pain does not require an obvious cause when trigeminal neuralgia strikes.
By contrast, the condition is not a dental problem, a sinus disorder, a stress-related complaint, or a psychological illness. Nor is it a pain condition that behaves predictably over time.
What happens in the nerve when trigeminal neuralgia strikes
The trigeminal nerve is not a single structure. Instead, it is a complex sensory network supplying the jaw, teeth, gums, cheeks, eyes and scalp.
When trigeminal neuralgia strikes, damage does not affect this network evenly. As a result, different nerve fibres misfire at different times. Consequently, pain may move location, change character, vary in severity, or appear without warning.
Uniform attacks would suggest uniform nerve damage. However, this is not how trigeminal neuralgia behaves biologically.
Why does pain change over time when trigeminal neuralgia strikes
Over time, repeated severe pain alters how the brain processes sensory signals. As this process develops, pain thresholds drop and incoming signals are amplified.
Because of this, when trigeminal neuralgia strikes later in the condition, people may experience longer attacks, background pain between attacks, or a shift in pain quality from sharp and electric to burning or crushing.
This progression is neurological. It is therefore not psychological, and it should never be dismissed as such.
Triggers when trigeminal neuralgia strikes: a medical clarification
Triggers do not cause trigeminal neuralgia. Rather, they activate an already irritable nerve.
Equally important, triggers are not required for an attack. For this reason, the absence of triggers should never be used to dismiss the diagnosis.
In practice, the same trigger may provoke pain one day and not the next. Avoiding triggers, therefore, does not mean the condition is controlled.
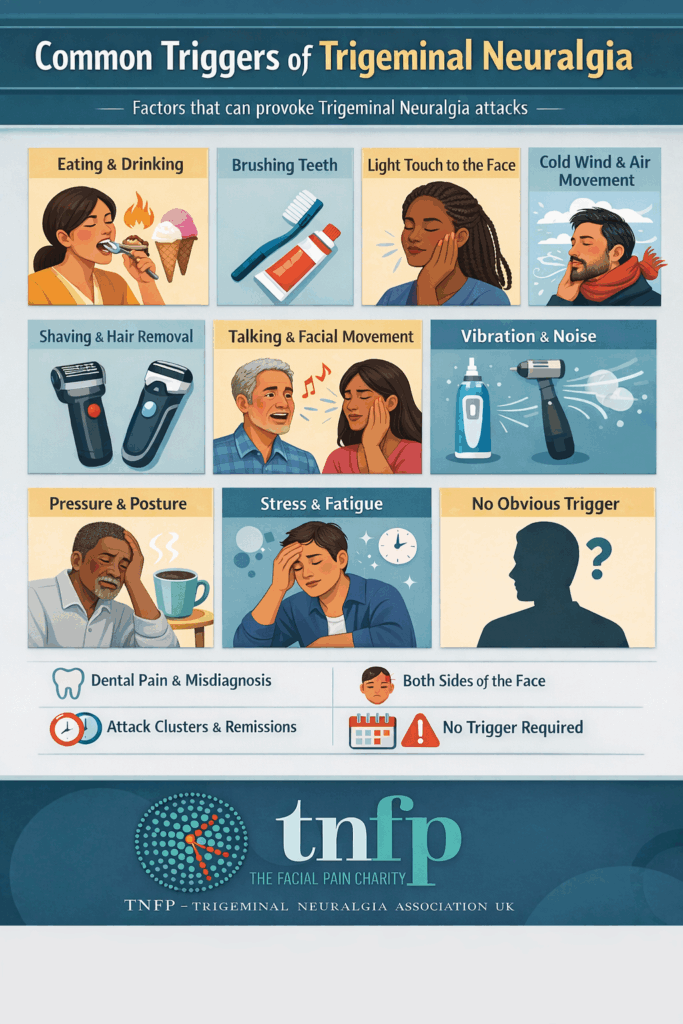
Common triggers when trigeminal neuralgia strikes
The following triggers are consistently recognised internationally when trigeminal neuralgia strikes. Importantly, not everyone experiences triggers, and trigger patterns may change over time.
Eating and drinking
Chewing, biting, swallowing and opening the mouth widely can all provoke pain. In addition, hard or crunchy foods, very hot or very cold food or drink, and spicy or acidic foods are commonly reported triggers.
As a result, repeated food-related attacks often lead to reduced intake and weight loss.
Brushing teeth and oral care
Brushing teeth, toothpaste or foam contacting the gums, flossing, mouthwash and dental instruments can all trigger attacks.
For this reason, pain triggered by brushing is a major cause of dental misdiagnosis and unnecessary procedures.
Light touch to the face
Washing the face, applying moisturiser or makeup, wiping the mouth, resting a hand on the face, or kissing may provoke pain.
Paradoxically, the lightest touch can trigger the most severe attacks.
Cold wind and air movement
Cold wind, air conditioning, fans and sudden temperature changes are well-recognised triggers.
Consequently, many people instinctively shield their face when trigeminal neuralgia strikes.
Shaving and hair removal
Shaving, electric razors, clippers, waxing or threading can activate sensitive nerve branches.
This applies to all genders and is frequently overlooked.
Talking and facial movement
Talking, prolonged conversation, smiling, laughing, yawning and chewing gum may provoke attacks.
In some cases, repeated movement leads to attack clusters rather than single episodes.
Vibration and noise
Electric toothbrushes, razors or clippers, dental drills and loud noise close to the face can trigger pain.
This reflects nerve reactivity, not psychological sensitivity.
Pressure and posture
Lying on the affected side, pressure from pillows, resting the face on a hand, or bending forward may worsen symptoms.
These triggers often fluctuate unpredictably.
Stress, fatigue, illness and hormonal change
Physical exhaustion, emotional stress, lack of sleep, infection, inflammation and hormonal fluctuation can all lower pain thresholds.
As a result, flare-ups often cluster during periods of physiological strain.
When trigeminal neuralgia strikes with no trigger at all
In some cases, when trigeminal neuralgia strikes, there is no identifiable trigger. Pain may occur at rest or during sleep.
This absence of triggers is one of the main reasons the condition is doubted or missed.
Why misdiagnosis happens when trigeminal neuralgia strikes
When trigeminal neuralgia strikes, pain frequently maps to teeth, jaw and sinuses. Consequently, people are often referred down dental and ENT pathways.
Normal scans can be misleading. As a result, years of unnecessary procedures are common before a correct diagnosis is made.
Patterns medicine still misunderstands when trigeminal neuralgia strikes
Attack clusters and remission
Trigeminal neuralgia often occurs in clusters, followed by periods of remission. However, remission does not mean resolution and does not rule out future flares.
Bilateral and alternating pain
The condition can affect both sides of the face. Pain may alternate sides or progress over time. Importantly, bilateral involvement does not exclude the diagnosis.
Why this matters
When variability is misunderstood, people are disbelieved. As a consequence, diagnosis is delayed, inappropriate procedures follow, and mental health deteriorates.
Changing pain does not mean changing illness. Instead, it reflects a complex neurological disorder behaving exactly as expected.
The clinical bottom line when trigeminal neuralgia strikes
Trigeminal neuralgia does not produce identical attacks because nerve damage is uneven, nerve firing is unstable, brain pain processing adapts over time, and physiological stressors fluctuate.
For these reasons, variability is not a diagnostic weakness. It is a diagnostic truth.
 References and clinical sources
References and clinical sources
-
NHS England
https://www.nhs.uk/conditions/trigeminal-neuralgia/ -
International Headache Society
https://ichd-3.org/ -
Cruccu G et al. Trigeminal neuralgia: new classification and diagnostic grading. Neurology.
-
Gronseth G et al. Practice guideline update: trigeminal neuralgia. Neurology.
-
Bendtsen L et al. Central sensitisation in neuropathic pain. Pain.
-
Woolf CJ. Central sensitisation and pain. Pain.